VOLUME 12 NUMBER 2 • NOVEMBER 2015
81
SA JOURNAL OF DIABETES & VASCULAR DISEASE
RESEARCH ARTICLE
= 0.007). The patients’ characteristics at rest were not statistically
significantly different (Table 2).
As shown in Table 3, peak systolic blood pressure was significantly
higher in G2 subjects than in G1 (213.6 ± 20.1 vs 200.0 ± 15.3
mmHg;
p
= 0.04). The difference between resting systolic and peak
systolic blood pressure (ΔSBP) as well as resting pulse pressure and
pulse pressure during exercise (ΔPP) followed a similar trend to that
of peak systolic blood pressure. Exercise capacity in G2 subjects was
significantly lower than in G1 by 12.94% (7.4 ± 1.1 vs 8.5 ± 1.5
METs;
p
= 0.042). Although, there was no statistically significant
difference between the LV mass index in the two groups, G2
subjects had significantly higher relative wall thicknesses than those
in G1 (0.53 ± 0.03 vs 0.41 ± 0.04;
p
< 0.001) (Table 4).
Discussion
The relationship of blood pressure response to exercise and
endorgan damage in hypertensive subjects is not clear. Studies on
this subject in diabetics are few, especially among blacks, who
unfortunately are at higher risk of developing cardiovascularrelated
complications than their Caucasian counterparts.
15
This study is the
first in Nigeria to assess the relationship between blood pressure
response to exercise and abnormal LV geometry.
In this study, gender, age and BMI were comparable among the
patients with normal LV geometry and those with LV concentric
remodelling. The longer duration of diabetes in patients with
concentric LV remodelling supports the earlier assertion that the
longer the duration of diabetes, the more the likelihood that the
patient will develop cardiovascular complications. This was despite
the fact that short-term (FBG, two-hour post-prandial blood
glucose) glycaemic control was similar in both groups in this study,
suggesting that blood pressure response during exercise may not
have been much influenced by blood glucose exposure.
It has been suggested that blood pressure response may be
related to blood glucose control.
16
Marfella
et al
. reported that
in the resting state, the presence of hyperglycaemia led to an
increase in SBP and DBP independently of endogenous insulin in 20
patients with type 2 diabetes. A reduced availability of nitric oxide
was suggested as a possible explanation.
16
In our study, the peak
systolic blood pressure during exercise was significantly higher in
patients with LV concentric remodelling than in those with normal
LV geometry. This however was not the case with peak diastolic
blood pressure. This was reflected in the significant change in pulse
pressure (ΔPP) observed during exercise. Pulse pressure provides a
crude guide to stiffness of the large conduit arteries.
17
Physiological
parameters related to blood pressure regulation and potential
contributors to reduced exercise capacity in type 2 diabetic
individuals include reduced LV systolic volume, altered myocardial
and diastolic functions and increased arterial stiffness.
5,18
The
elevated peak exercise SBP observed in patients with concentric left
ventricular remodelling in this study was probably partly associated
with arterial stiffness, as reflected by the higher ΔPP.
5,6
Exercise capacity was also reduced in patients with LV concentric
hypertrophy in our study. This may provide additional explanation
for reduced exercise tolerance in normotensive diabetes patients. It
has been suggested that the voltage on the ECG of left ventricular
hypertrophy may be an early marker of impaired exercise capacity.
19
Previous studies have shown that left ventricular hypertrophy
independently predicted reduced exercise capacity.
20
This study has
shown that type 2 diabetic patients with increased peak systolic
blood pressure had increased arterial stiffness, higher LVMI,
abnormal LV geometry and reduced exercise capacity.
Conclusion
Normotensive diabetics with concentric left ventricular remodelling
have increased systolic blood pressure reactivity to exercise. It is
probable, as suggested in earlier studies, that increased blood
pressure reactivity to exercise is an indicator of target-organ
damage, especially in normotensive diabetics.
References
1. Gottdierer JS, Brown J, Zoltick J, Fletcher RD. Left ventricular hypertrophy in men
with normal blood pressure: relation to exaggerated blood pressure response to
exercise.
Ann Intern Med
1990;
112
: 161–166.
2. Al’Absi M, Devereux RB, Lewis CE,
et al
. Blood pressure responses to acute stress
and left ventricular mass.
Am J Cardiol
2002;
89
: 536–540.
3. Rostrup M, Smith G, Bjo¨ rnstad H, Westheim A, Stokland O, Eide I. Left ventricular
mass and cardiovascular reactivity in young men.
Hypertension
1994;
23
(Suppl I):
I168–I171.
4. Stewart KJ, Sung J, Silber HA,
et al.
Exaggerated exercise blood pressure is related
to impaired endothelial vasodilator function.
Am J Hypertens
2004;
17
(4): 314–
320.
5. Devereux RB, Roman MJ, Paranicas M,
et al.
Impact of diabetes on cardiac
structure and function: the Strong Heart Study.
Circulation
2000;
101
: 2271–
2276.
6. Chen CH, Nakayama M, Nevo E, Fetics BJ, Maughan WL, Kass DA. Coupled
systolic-ventricular and vascular stiffening with age: implications for pressure
regulation and cardiac reserve in the elderly.
J Am Coll Cardiol
1998;
32
: 1221–
1227.
7. Berne RM, Levy MN. Peripheral circulation and its control.
Physiology
, 4th edn.
Sydney: Mosby, 1998, Vol. 1: 1130.
8. World Health Organization. Second Report of the Expert Committee on Diabetes.
Geneva. World Health Org, 1980; (Tech Rep Ser 646).
9. Bruce RA. Exercise testing of patients with coronary disease. Principles and normal
standards for evaluation.
Ann Clin Res
1971;
3
: 323–332.
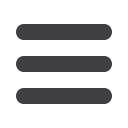
Table 3.
Exercise-induced haemodynamic factors
Parameters
Normal LV
geometry
(
n
= 19)
Concentric
LV remodelling
(
n
= 11)
p
-value
(Student’s
t
-test)
pHR (bpm)
167.8 ± 10.9 162.8 ± 21.7
0.405
pDBP (mmHg)
94.2 ± 7.7
98.2 ± 11.7
0.270
pSBP (mmHg)
200.0 ± 15.3 213.6 ± 20.1
0.045
ΔHR (bpm)
75.7 ± 18.4 72.7 ± 28.1
0.725
ΔDBP (mmHg)
21.5 ± 14.1 24.0 ± 13.3
0.596
ΔSBP (mmHg)
81.5 ± 14.1 98.9 ± 20.1
0.010
ΔPP (mmHg)
105.8 ± 9.6 115.5 ± 11.3
0.019
HR reserve
0.97 ± 0.16 0.87 ± 0.03
0.222
Exercise capacity (METs)
8.5 ± 1.5
7.4 ± 1.1
0.042
Statistical significance at p < 0.05
Values are expressed as mean ± SD.
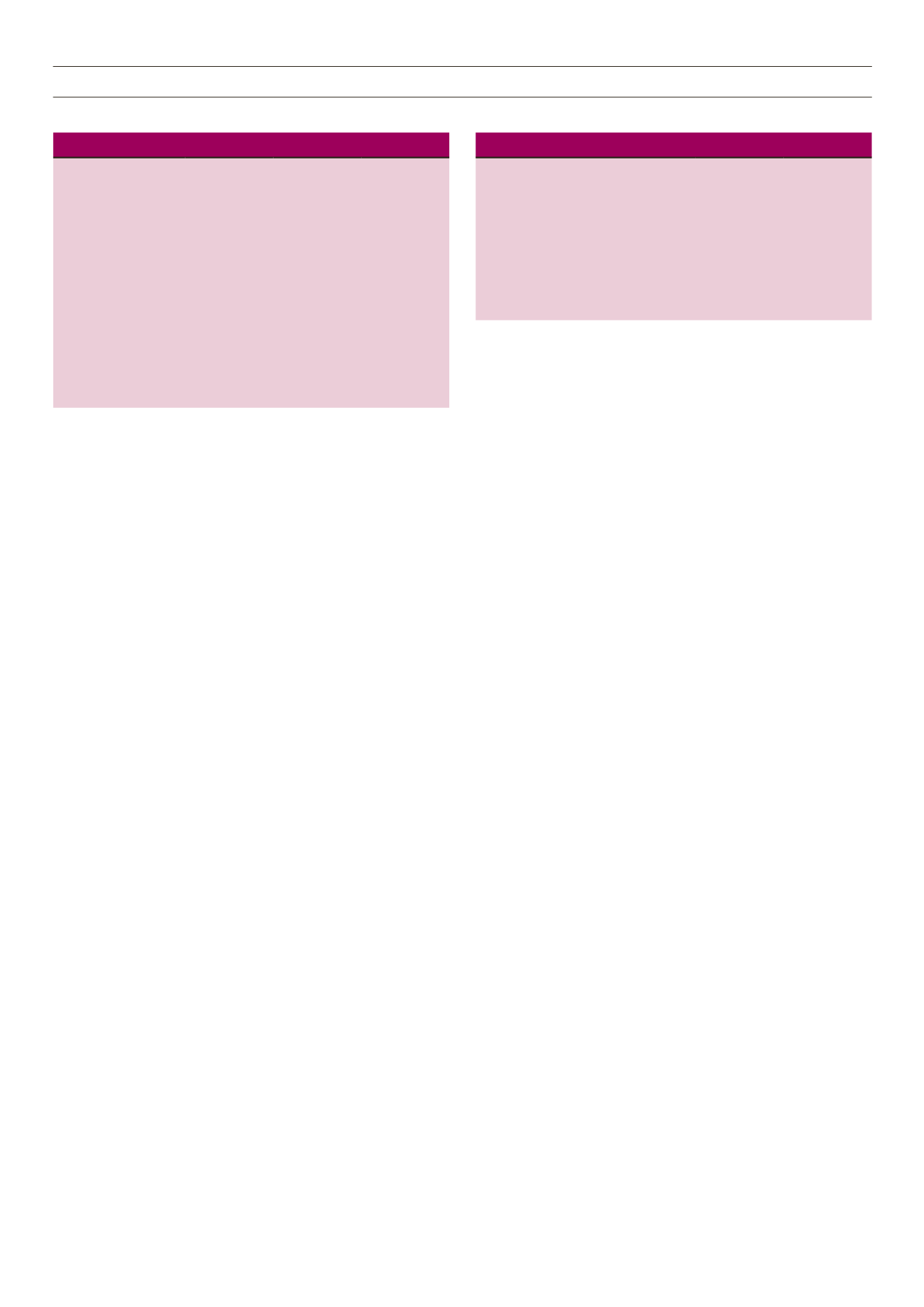
Table 4.
Echocardiographic parameters of G1 and G2 subjects
Parameters
Normal LV
geometry
(
n
= 19)
Concentric
LV remodelling
(
n
= 11)
p
-value
(Student’s
t
-test)
LVMI (g/m
2
)
81.1 ± 13.4 88.9 ± 21.8
0.233
IVST (mm)
9.8 ± 1.2
11.1 ± 1.3
0.010
PWT (mm)
9.0 ± 1.3
10.9 ± 1.1
< 0.001
RWT
0.41 ± 0.04 0.53 ± 0.03
< 0.001
Statistical significance at
p
< 0.05
Values are expressed as mean ± SD.



















